Heat stress
Heat stress occurs when the body is unable to cool itself fast enough to maintain a safe internal (core) temperature of around 37°C.
This page has information about how heat affects the body, how to identify risks and what to do about them. It also includes information on training for workers and managers, first aid and emergency procedures.
When core temperature rises above this level, the body is put under strain which can lead to heat-related illness (or even death in severe cases).
In the workplace, a worker’s ability to maintain a safe core temperature is influenced by three main factors:
- individual and pre-disposing factors
- the conditions in the work environment
- the type of work being undertaken.
The Heat stress (basic) calculator is a simple online tool designed for use by anyone with basic knowledge of the work area and process. There is no direct measurement of environmental conditions required to use the calculator.
Most people feel comfortable when the air temperature is between 20°C and 27°C and when the relative humidity ranges from 35 to 60 per cent.
People may feel discomfort when air temperature or humidity is higher than this. However, it is important to note that such situations do not cause harm as long as the body can adjust and cope with the additional heat.
The body’s normal response to an elevated core temperature include:
- vasodilation (widening of blood vessels)
- sweating
- increased respiratory rate
- increased heart rate.
When the body is unable to cool itself effectively and maintain a normal core temperature, risk of developing one or more of the following illnesses is possible:
Heat rash – sometimes called 'prickly heat'. It is a skin irritation caused by excessive sweating and:
- can occur at any age
- is most commonly associated with humid /dusty tasks in which the skin pores become blocked
- looks like a red cluster of pimples or small blisters
- is most likely to occur on the neck and upper chest, and in skin folds and creases.
Heat cramps – these include muscle pains or spasms, usually in the abdomen, arms or legs. They may occur after strenuous activity in a hot environment, when the body gets depleted of salt and water. They may also be a symptom of heat exhaustion.
Dizziness and fainting – heat related dizziness and fainting results from reduced blood flow to the brain. Heat causes an increase in blood flow to the skin and pooling of blood in the legs, which can lead to a sudden drop in blood pressure.
Heat exhaustion – is a serious condition that can develop into heatstroke. It occurs when excessive sweating in a hot environment reduces the blood volume. Warning signs may include paleness and sweating, rapid heart rate, muscle cramps (usually in the abdomen, arms or legs), headache, nausea and vomiting, dizziness or fainting.
Heatstroke – is a medical emergency and requires urgent attention. Heatstroke occurs when the core body temperature rises above 40.5 °C and the body's internal systems start to shut down. Many organs in the body can suffer damage and to rectify it, the person's body temperature must be reduced quickly. Most people will have profound central nervous system changes such as delirium, coma and seizures. The person may stagger, appear confused, have a fit or collapse and become unconscious. As well as effects on the nervous system, there can be liver, kidney, muscle and heart damage. The symptoms of heatstroke may be the same as for heat exhaustion, but the skin may be dry with no sweating and the person's mental condition worsens.
Heatstroke requires immediate first aid and medical attention.
Delayed treatment may result in death. Watch the film A Current Affair - Melting Man, which outlines the tragic consequences that can occur if heat strain factors are not adequately controlled.
Heat hangover – While incidents of heat stroke are rare, mild to moderate symptoms of heat exhaustion and less severe incidents of heat related illnesses (including heat rash, syncope and cramps) are more common and typically present as ad-hoc individual events during the summer. In addition, workers often describe experiencing fatigue-like symptoms after being repeatedly exposed to moderate to high heat conditions for prolonged periods. These unpleasant physiological and psychological side effects have been referred to as ‘heat hangovers’ which can manifest as irritability, headaches, nausea, loss of appetite and general lethargy towards the end of shift and/or following shift. Based upon preliminary evidence in other outdoor industries located in Queensland, it appears the hangovers do not require excessively high core body temperatures. Rather, moderate body temperatures for extended periods, likely in excess of an individual’s capacity, appear to precipitate the hangovers [1].
The impact of heat exposure on workers can affect physical and mental performance and this may contribute indirectly to an increase in safety related incidents. For example, the performance of complex tasks (which require greater concentration and manipulation) may be adversely impacted when mental and physical impairment occurs as a result of heat exposure. Increased trends in incidents of work-related injury have coincided with elevated ambient temperatures and the warmer summer months of the year [2]. Furthermore, the impacts of heat wave events have reportedly resulted in a 45% increase in workers compensation claims within the Brisbane region [3].
[1] Preliminary evidence of a heat hangover, a new heat illness classification for occupational settings? Brearley, M. Townsville : Conference: Science of Sport, Exercise and Physical Activity in the Tropics, 2016
[2] Are workers at risk of occupational injuries due to heat exposure? A comprehensive literature review. Varghese, B M, et al. 2018, Safety Science, pp. 110: 380-392.
[3] Characterising the impact of heatwaves on work-related injuries and illnesses in three Australian cities using a standard heatwave definition- Excess Heat Factor (EHF). Varghese, B M, et al. 2019, Journal of Exposure Science and Environmental Epidemiology, pp. (29) 821-830.
Further information
For more information, visit Heat hangover | ThermalHyperformance.
Under section 42 of the Work Health and Safety Regulation 2011 (WHS Regulation), PCBU’s have a duty to provide first aid. Where risk of heat stress exists in a workplace, first aid needs to be suitable for the work environment and the nature of the work.
The Australian and New Zealand Committee on Resuscitation (ANZCOR) provide guidance on suitable first provisions for heat related illness.
Guideline 9.3.4 – Heat Induced Illness (Hyperthermia)
Heat stroke is a life threatening emergency. In workplaces where this risk exists, emergency management plans (developed in accordance with section 43 of the WHS Regulation) need to include:
- emergency procedures in the event of heat stroke including details of medical treatment and assistance, and
- information, training, and instruction to relevant workers in relation to implementing the emergency procedures.
There is no workplace exposure standard or limit for heat stress. Heat stress indices are not safe/unsafe limits and should only be used as guides.
Setting of a safe/unsafe limit simply based on ambient air temperature is not appropriate due to the many variables (task, environment and individual) associated with the onset of heat strain.
Managing heat stress begins with proper identification and assessment—remember it’s not just about the air temperature.
There are three main factors to consider when identifying risk of heat stress.
- Environmental factors including ambient temperature, relative humidity, radiant heat, and wind speed.
- Work process factors including the type of work being undertaken, the duration and timing of exposure, work intensity, and the type of clothing and protective gear used.
- Individual factors include acclimatisation, health and hydration levels, physical fitness, age, fatigue, and certain medications.
It is important to involve your workers when identifying heat stress issues and possible solutions.
You should also consider any previous heat related incidents or complaints.
Identification and assessment
Identifying and managing heat stress is not just about the air temperature.
Assessing risks of heat related illness requires accurate identification and assessment of:
- workplace conditions
- job requirements.
- individual worker attributes.
Conduct a walk-through survey of the workplace and ask your workers about their heat stress issues. Consider the work location's previous history of heat stress issues, including what time of day or year and under what circumstances they occurred.
Heat stress risk assessment flow chart
Use the following three level approach to identify heat stress factors in your workplace (Di Corleto et al 2013).
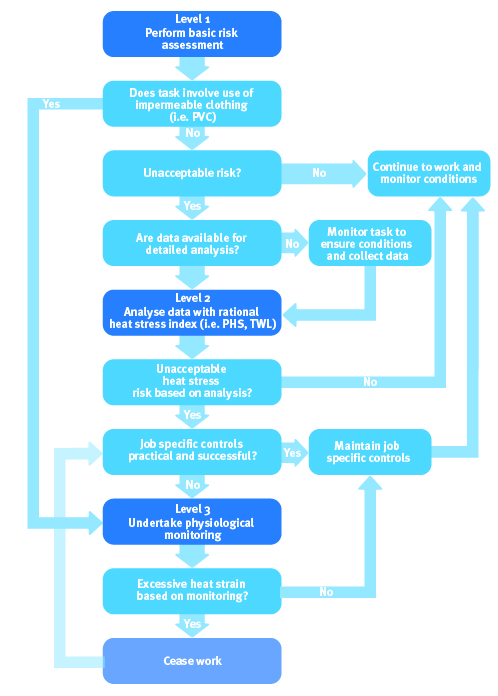
Level 1 (Non-technical): is a basic risk assessment, which can use a simple index such as the Heat stress (basic) calculator.
Heat stress (basic) calculator is a simple online tool designed for use by anyone with basic knowledge of the work area and process. There is no direct measurement of environmental conditions required to use the calculator.
The online calculator uses a number of factors to make a basic assessment of heat stress including:
- the state of acclimatisation
- work demands, location
- clothing
- sun exposure
- hot surfaces
- task complexity
- air movement, and other factors
- apparent temperature (this is calculated using ambient temperature and relative humidity).
NOTE: As the basic assessment is a qualitative assessment, instrumentation for measurement of wet bulb glove temperature (WBGT) is not mandatory meaning people with limited technical expertise and equipment can identify and assess the risk factors. The basic assessment can therefore be performed using readily available information at the workplace (i.e. ambient air temperature and relative humidity).
The online calculator is an initial qualitative review of potential heat stress situations and is not a definitive assessment tool.
A level 2 (technical) assessment will be needed when the online calculator identifies an unacceptable level of heat stress risk.
Level 2 (Technical): needs additional data collected and the use of a second level index such as ISO 7933: Predicted Heat Strain (PHS) or Thermal Work Limit (TWL). A range of measuring equipment and expertise is required for this type of assessment.
Additional data needed for this type of assessment will include:
- dry bulb temperature
- globe temperature
- air velocity
- humidity
- metabolic load
- clothing type
- posture.
This type of assessment and gathering of required data should only be undertaken by a competent person such as an occupational hygienist or occupational physician.
The University of Queensland (UQ) has developed a smart phone app based on ISO 7933, called PHS, visit The Thermal Environment for more information.
A level 3 (expert) assessment will be needed when either:
- data cannot be collected
- where impermeable clothing is used.
Level 3 (Expertise): Physiological monitoring
Physiological monitoring is used in cases of high heat stress risk such as:
- work involving the use of encapsulating suites (e.g. hazmat suits) or high levels of external PPE
- environments where the level 2 assessment indicates allowable exposure times of less than 30 minutes
- where a work environment cannot be accurately assessed.
The risk and severity of heat related illness will vary widely among workers, even under identical heat stress conditions. Individual monitoring measures a worker's physiological responses (such as elevated body temperature and/or heart rate) to assess the effectiveness of implemented controls.
Control the risks
There are two approaches to controlling the risk:
- modify the environment to suit the work
- modify work to suit the environment.
Look carefully at the control measures that can be used, some are more practical for certain situations than others. In most situations, multiple controls from the following will be required.
Modifying the environment to suit the work
Control the source of the heat
- Reduce the temperature of the source of heat (e.g. allow the section of plant or equipment to cool before work commences).
- Insulate hot surfaces (can also provide protection from contact burns).
- Clad or cover sources of radiant heat.
- Use radiant heat shields or barriers (need to have good insulation properties and low emissivity/high reflectivity so they don't become hot).
- Use shade barriers (e.g. temporary gazebos) over the work area to block heat from the sun.
Ventilation, air conditioning and air movement
- Remove or dilute hot/humid air and replace it with cooler/drier air. This is the most efficient method and can be achieved by either forced mechanical ventilation or naturally. It is especially important in hot and humid environments. Examples include:
- mechanical ventilation which draws cool air from outside the work area to displace the hotter air
- exhaust or extraction fans to remove hot air
- natural ventilation via windows, doors and roof vents/louvres
- Increase air movement in the work area e.g. fans.
- Use artificial cooling such as evaporative coolers, air conditioning, vortex tubes, or chillers.
Modifying the work to suit the environment
Modify the work process
- Use mechanical aids such as cranes, forklifts and earthmoving plant to reduce the workload.
- Conduct work at ground level or organise work to minimise climbing up and down stairs and ladders.
- Do the work indoors or in a shaded area.
Provide rest areas/refuges to escape the heat
- Use refuges for workers to escape the effects of hot environments.
- Locate as near to the work area as possible.
- Provide shelters (shelters can range from temporary gazebos through to insulated structures or cabins which are air-conditioned.
Administrative controls
- Worker selection – workers who have become acclimatised to the work environment are at less risk than unacclimatised workers.
- Scheduling of work – where possible, conduct the work:
- in cooler parts of the year, especially where the work requires protective clothing
- at night, early morning or late afternoon rather than midday.
- Work-rest intervals:
- spend rest periods in a cool place with a plentiful supply of cool water for fluid replacement.
- remove protective clothing during breaks to allow workers to cool off.
- Fluid replacement – critical when working in a hot environment, especially where hard work (metabolic work) is required:
- drink small volumes as frequently as possible during work
- provide cool drinks or water as close as possible to the work area (if supplying drinks, make sure the workers actually like them)
- help workers to self-monitor their hydration status via hydration test strips and urine colour charts
- encourage workers to avoid diuretic drinks immediately prior to starting work and to rehydrate between shifts
- encourage workers to consume water at the start of the shift so as to maximise their hydration status
- encourage the replacement of electrolytes in high sweat scenarios.
- Buddy systems – trained workers can keep an eye on each other for signs of heat effects, reducing risks compared to isolated workers.
Personal protective equipment (PPE)
Clothing and particularly protective clothing can often have an adverse effect on the body's heat balance in hot environments by insulating the body and reducing evaporative heat loss. Impervious clothing can impede heat loss.
PPE can also help to reduce the risk of heat strain in some circumstances.
Examples include:
- wearing a hat to protect from sunlight
- vented safety eye wear (where safe to do so)
- protective clothing (especially if made from natural fibre, will provide some protection against contact burns and radiation)
- wearing light coloured (especially white, and reflective clothing e.g. aluminised) which absorb comparatively little radiant heat energy
- respiratory protective equipment (RPE) with an exhalation valve
- wearing cotton gloves as a lining under regular gloves
- wearing lightweight/cotton undergarments
- using specialised cooled or conditioned personal protective clothing including:
- air circulating systems: these usually incorporate the use of a vortex cooling tube. Depending on the size of the vortex tube, they may be used to cool a large volume system such as a tank or may be utilised as a personal system whereby the vortex is worn on the belt and cool air is fed into an air supplied helmet and/or vest (e.g. powered air purifying respirators (PAPR)). Breathing quality air should only be used for such air -supplied systems
- liquid circulating systems: these systems rely on the principle of heat dissipation by transferring heat from the body of the liquid and then the heat sink (which is usually an ice water pack). Liquid (water) cooling suits must be worn close to the skin and the chilled liquid is pumped through fine capillary tubing from either a battery powered pump worn on the belt or through an 'umbilical cord' from a remote cooling unit
- ice cooling systems: these involve the placement of ice or other materials such as n-tetradecane in pockets in an insulating garment, typically a vest, worn close to the skin such that heat is conducted away. This in turn cools the blood in the vessels close to the skin surface, which then helps lower the core temperature
- reflective systems: reflective clothing is utilised to help reduce radiant heat load on an individual. It acts as a barrier between the person's skin and the hot surface reflecting away the infrared radiation. The most common configuration of reflective clothing is an aluminised surface bonded to a base fabric.
Note: Long work clothing is not a cause of heat related illness. Rather multiple factors, as outlined above, collectively cause heat related illness. Outdoor workers should wear long pants and work shirts with a collar and long sleeves to cover as much skin as possible. This is because outdoor workers are exposed to high levels of direct sunlight over long periods of time, generally receiving five to 10 times more ultraviolet radiation exposure per year than indoor workers. Therefore, outdoor workers are at an increased risk of skin cancer and other health issues related to excess UV radiation.
Read more about sun safety for outdoor workers
Training
Training is required for all workers likely to be working in hot environments, undertaking strenuous work at elevated temperatures and those who wear impermeable protective clothing.
Training should include:
- mechanisms of heat exposure
- potential heat exposure situations
- recognition of predisposing factors
- importance of fluid intake
- the nature of acclimatisation
- effects of alcohol and drugs
- early recognition of symptoms of heat illness
- prevention of heat illness
- first aid treatment of heat illnesses
- self-assessment (this is a critical key element)
- how medical surveillance programs work and the advantages of employee participation.
Use the Heat stress (basic) calculator as part of training by encouraging your workers to input combinations of different controls to achieve an improved risk score.
A Current Affair - Melting Man
This story shows the tragic consequences that can occur if heat strain factors are not adequately controlled. Story provided to Workplace Health and Safety Queensland courtesy of the Nine Network's A Current Affair program.
Download a copy of this film (MP4, 221MB)
eSafe articles
- Heat stress – know the facts to protect your workers
- Protect your workers from summer heat stress (Jan 2024)
- Heat-related illness
- Protect your workers from summer heat stress (Nov 2023)
- Extreme weather and heat stress
- Avoiding heat stress
- Heat stressing you out already?
- Formwokers suffer heat stress
- SafeWork South Australia – Heat awareness
Other resources
- AIOH – A guide to Managing Heat Stress: Developed for Use in the Australian Environment
- ISO 7933:2004 Ergonomics of the thermal environment - Analytical determination and interpretation of heat stress using calculation of the predicted heat strain.
- W502 Student Manual: Thermal Environment. February 2016. Occupational Hygiene Training Association. The Thermal Environment
- Heat stress (basic) calculator